Diagnosis is a crucial step in the treatment of any mental illness. It should be detailed, accurate, and provide reassurance. The classification and diagnosis of schizophrenia is thus a crucial step in the treatment of schizophrenia, and various classification systems are used by psychologists. What are the different diagnosis and classification tools used in schizophrenia? How do they differ?
Let's explore the two most well-known classification manuals in psychology, the ICD (International Classification of Diseases) and the DSM (Diagnostic and Statistical Manual of Mental Disorders), and how the two differ in their approach to schizophrenia.
- We will discuss the classification and diagnosis of schizophrenia, paying particular attention to the ICD (International Classification of Diseases) and the DSM (Diagnostic and Statistical Manual of Mental Disorders).
- We will then go on to discuss the types of schizophrenia.
- Following this, we will highlight the symptoms of schizophrenia, including the positive symptoms of schizophrenia and the negative symptoms of schizophrenia.
- We will also cover the causes of schizophrenia.
- Finally, we will describe and evaluate the classification and diagnosis of schizophrenia, discussing the problems with using classification tools in diagnosis.
Diagnosis of Schizophrenia
Both the ICD (International Classification of Diseases) and the DSM (Diagnostic and Statistical Manual of Mental Disorders) provide a way to classify psychiatric disorders. It refers to grouping symptoms based on how they usually present in disorders. This classification allows for a diagnosis.
Depending on which manual a clinician or psychiatrist uses, a diagnosis and classification of schizophrenia essentially refer to a person having a mental illness affecting their thoughts, feelings, and speech, causing a loss of contact with the self and a sense of reality.
Typically, schizophrenia affects:
- People between the ages of 15 and 45.
- More men than women.
- More people in cities.
- More people from lower economic backgrounds or groups.
What is the ICD (International Classification of Diseases)?
The ICD is a classification manual used in most countries of the world (especially in Europe) to diagnose psychiatric disorders.
It is currently in its eleventh edition and has undergone several revisions.
These revisions focus on improving the reliability and validity of the classification tool.
According to the ICD, for a patient to be diagnosed with schizophrenia:
The DSM is sometimes still used as the basis for the ICD.
What is the DSM (Diagnostic and Statistical Manual of Mental Disorders)?
The DSM is a classification manual similar to the ICD, though it is used primarily by American medical professionals. The American Psychiatric Association (1980) developed it and is currently in its fifth edition, which has also been revised to improve reliability and validity.
Similar to the ICD, to receive a diagnosis of schizophrenia, a patient must meet the following requirements:
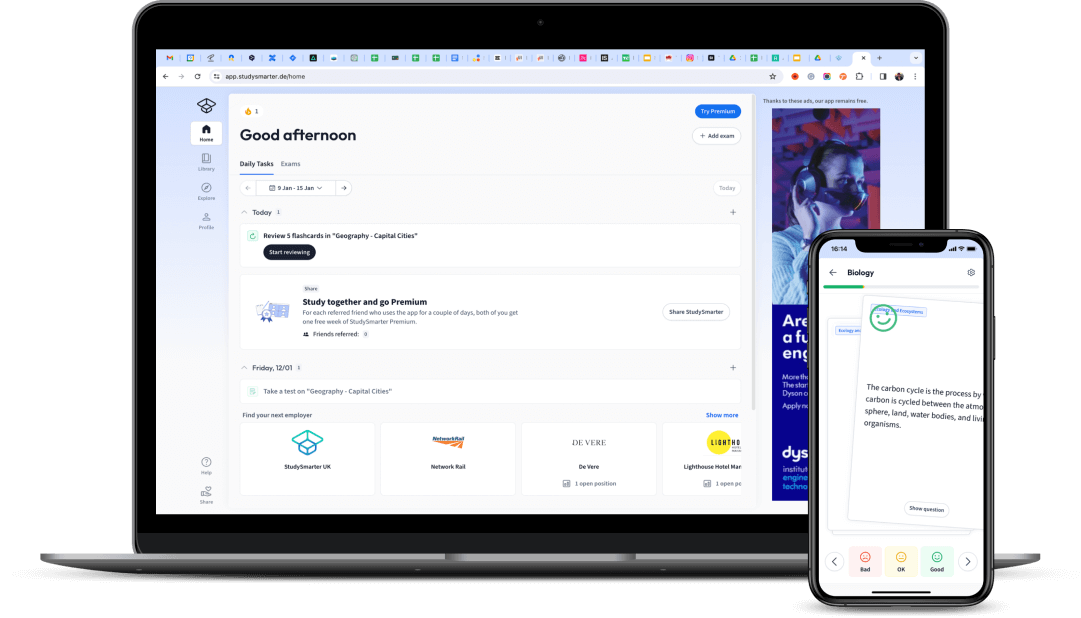
 Fig. 1 - Speaking with a professional can help people diagnose their mental health issues, Canva.
Fig. 1 - Speaking with a professional can help people diagnose their mental health issues, Canva.
What are the types of schizophrenia?
The following is not particularly relevant to the exam, but it is helpful to know the history of the disease.
The types of schizophrenia vary depending on the diagnostic manual you follow. The latest version of the DSM no longer has types (something to keep in mind), but some still refer to them. In general, these are the types you may be diagnosed with:
Paranoid Schizophrenia.
Catatonic Schizophrenia.
Schizoaffective disorder.
Disorganised Schizophrenia.
Residual Schizophrenia.
Undifferentiated Schizophrenia.
Famously, Bleuler established the four A's of schizophrenia (McNally, 2009):
Affect blunting.
Alogia.
Ambivalence.
Autism.
What are the Symptoms of Schizophrenia?
Symptoms can be divided into two categories:
Positive.
Negative.
Here are examples of positive and negative symptoms of schizophrenia.
What are the Positive Symptoms of Schizophrenia?
Positive symptoms can be described as symptoms that add an experience for an individual. What we mean by this is that the symptom is causing an additional experience that changes a patient's perception.
Positive symptoms are when symptoms are adding an experience to a patient's life, causing a change in behaviour. Typically, they cause reality perception problems.
For example:
Hallucinations: A sensory experience, usually auditory or visual, although not exclusively. Patients can:
See distortions, such as seeing lights and patterns that are not there.
See objects that look like faces.
Hear voices outside their head that are not their own, telling them to do things.
Delusions: Irrational beliefs and thoughts that can manifest in multiple ways:
Disorganised speech: Disjointed sentences, changing the subject in the middle of a sentence without thinking about it.
Psychomotor disturbances: Rocking back and forth for long periods, which may alternatively manifest as catatonia (holding still for hours or days).
What are the Negative Symptoms of Schizophrenia?
Negative symptoms are the opposite of positive because they take something away from the patient. In essence, it is a loss of functioning.
Negative symptoms of schizophrenia remove experiences from a patient, usually through withdrawing from their world and losing the ability to remain involved.
Here are some examples:
Alogia (speech poverty) refers to a decrease in the quality and quantity of speech. Patients speak slower, less, and delay their responses. (If it is too disorganised, it becomes a positive symptom in the DSM-V, as mentioned above).
Classifying disorders allows clinicians to discuss patients and their symptoms and creates a consensus for effective, standardised treatment.
Without the guidelines in these manuals, disorders would not be formally recognised. A patient in one part of the world might receive a completely different diagnosis, and therefore different treatment than a patient in another part of the world.
Therefore, it is essential to assess the reliability and validity of the classification systems and the consistency of the diagnoses. It is also essential to understand the implications of using such a system to 'pigeonhole' patients.
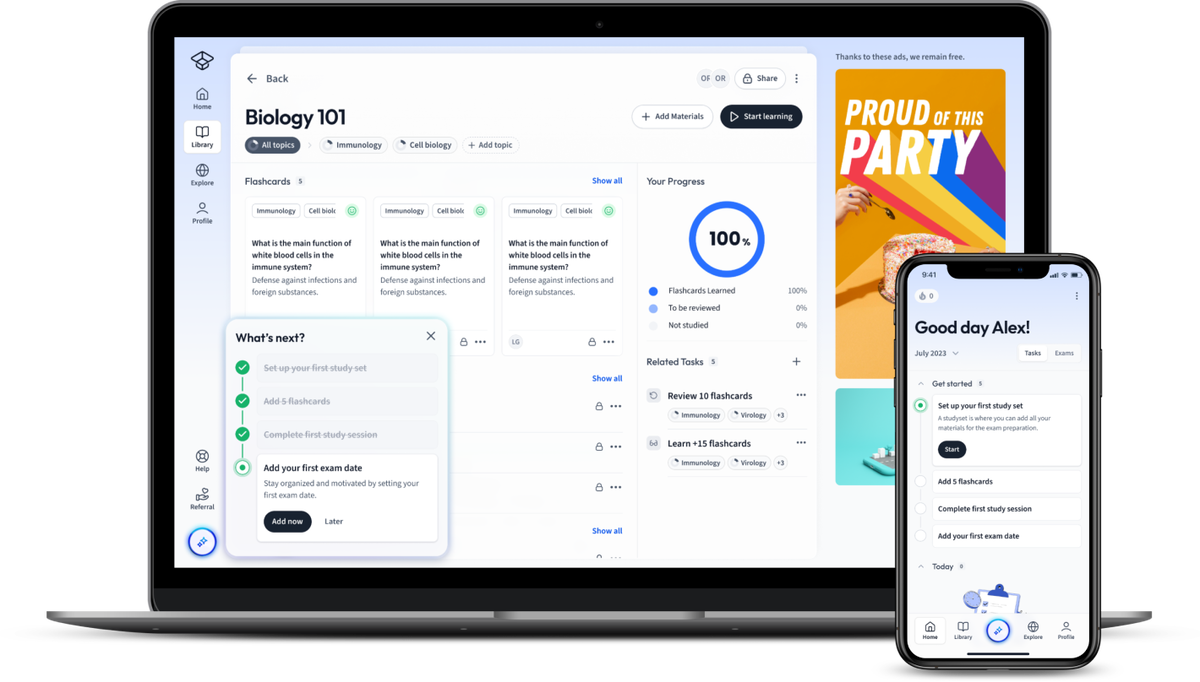
 Fig. 2 - Positive and negative symptoms of schizophrenia differ.
Fig. 2 - Positive and negative symptoms of schizophrenia differ.
The role of dopamine dysfunction in schizophrenia is essential, as dopamine is one of the primary neurotransmitters associated with the disorder. The dopamine hypothesis looks at this issue more in-depth.
Causes of Schizophrenia
There are various arguments out there that discuss the causes of schizophrenia, and they tend to fall into two categories:
- Biological explanations of schizophrenia
- Psychological explanations of schizophrenia
Biological explanations for schizophrenia attribute the cause of the disorder to neural correlates, brain abnormalities, genetics, and the dopamine hypothesis.
Psychological explanations for schizophrenia focus more so on family dysfunctions and cognitive explanations.
Describe and Evaluate the Classification of Schizophrenia
It is worth briefly pointing out the general problem of using a classification system to 'label' patients with disorders, as we need to evaluate the classification and diagnosis of schizophrenia.
Advocating the idea that schizophrenic patients are ‘dangerous' had a strong emotional impact on the way people react emotionally to someone with schizophrenia. Calling them needy led to mixed reactions.
In comparison, people with major depression were not as stigmatised in public opinion.
- Scheff (1999) also considered that mental illness labelling profoundly affected the stigmatised patients and almost created a self-fulfilling prophecy, i.e. patients began to behave as they were 'expected' to as schizophrenic or mentally ill people after being labelled.
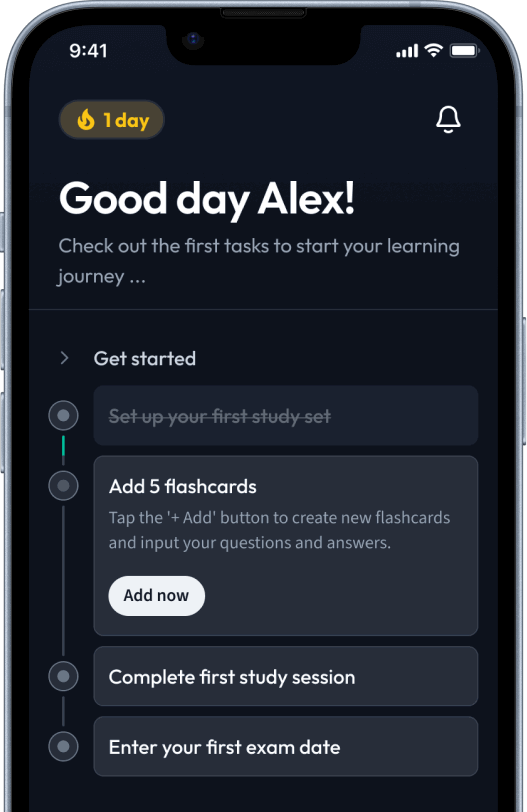
 Fig. 3 - Schizophrenia labels often come with stigma.
Fig. 3 - Schizophrenia labels often come with stigma.
When two different classification systems are used, problems with reliability and validity arise in diagnosing schizophrenia. When two classification systems are used to diagnose a disorder, clinicians may not agree on a diagnosis because one manual may not list the same symptoms as another manual.
How can a person reliably diagnose schizophrenia when the ICD states to look for one set of symptoms, and the DSM states to look for a different set of prioritised symptoms?
If a person is misdiagnosed, the treatment may not be effective and address the root cause of the symptoms directly. It would be best to keep that in mind when consulting these diagnostic and classification tools.
Issues with comorbidity also exist, in that there is not enough separation between symptoms of different mental disorders.
Diagnosis and Classification of Schizophrenia - Key Takeaways
- The main classification tools used by professional diagnosticians are ICD (International Classification of Diseases) and the DSM (Diagnostic and Statistical Manual of Mental Disorders). The ICD is used worldwide, while the DSM is mainly used in America.
- The ICD and the DSM go through revisions to improve the reliability and validity of their manuals. For schizophrenia, they require positive and negative symptoms, and both must last at least one month for a diagnosis.
- Schizophrenia has positive and negative symptoms. Positive symptoms give the patient new, additional experiences in their perception of reality, whilst negative symptoms take experiences away from the patient.
- Classification tools are essential so that doctors worldwide can make consistent diagnoses. Two patients with the same condition could receive different diagnoses and treatments from different doctors without them.
- There is a problem of stigma when using classification tools. The labelling of a mental illness, especially schizophrenia, in some cases leads to stereotyping and negative public attitudes.
Explanations
Exams
Magazine