We all know what stress feels like, but have you ever wondered what happens inside your body when stressed? How does our body prepare us to handle the stressors we encounter in life? Maybe you have read about the fight-or-flight system, but there is more to learn about the body’s stress response.
- First, we will explore the function of the hypothalamic-pituitary-adrenal (HPA) system.
- Next, we will look at abnormalities in the HPA system.
- We will look at the HPA system and depression.
- Then, we will examine the HPA system and stress.
- Finally, we will discuss the effects of HPA system dysfunction.
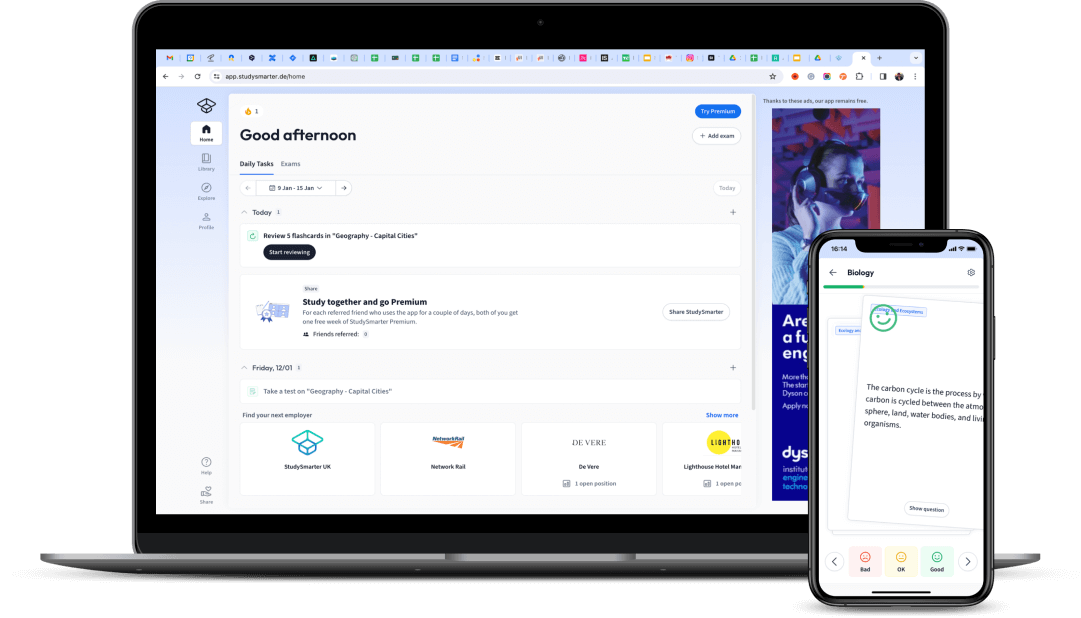
 Fig. 1 - Stress can not only have a psychological effect on you but a physiological one too.
Fig. 1 - Stress can not only have a psychological effect on you but a physiological one too.
Hypothalamic-Pituitary-Adrenal System: Function
Several areas of the brain connect to each other and work together in our response to stress. The hypothalamic-pituitary-adrenal system (HPA axis) is the body’s response system to chronic stress (long-term stress). The HPA axis does not react as fast as the sympathomedullary pathway, the body’s response to acute stress.
The HPA axis consists of the hypothalamus, the pituitary gland, and the adrenal gland.
Here is an overview of the HPA axis and how it functions:
Stages ofthe HPA-Axis Process | What happens during this stage? |
| Stage 1: Initial Response | The hypothalamic-pituitary-adrenal system kicks in after the initial fight or flight response. If a person experiences prolonged stress, the hypothalamus is activated. As a result, a chemical messenger corticotropin-releasing hormone (CRH) is released into the bloodstream. |
| Stage 2: Pituitary Gland | CRH causes the anterior pituitary gland (situated just above the brainstem) to produce and release adrenocorticotropic hormone (ACTH), transported to the adrenal glands. |
| Stage 3: Adrenal Gland | The adrenal cortex (the outer region of the adrenal glands) is stimulated to produce cortisol. |
| Stage 4: Energy Conversion | Cortisol converts protein into glucose, releasing a steady supply of blood sugar, providing a constant stream of energy and allowing the person to deal with the stressor.Cortisol also results in - Lowered pain sensitivity.
- Lowered immune response.
- Diminished cognitive functions such as concentration.
- Slowing down digestion.
|
| Stage 5: Homeostasis Returns | The hypothalamic-pituitary-adrenal system is self-regulating via a ‘negative feedback loop’. The brain monitors the cortisol levels; if high levels are detected, the levels of CRH and ACTH decrease, leading to a reduction of cortisol levels. |
This 5 stage process takes about 20 minutes.
Hypothalamic-Pituitary-Adrenal System: Abnormality
Barring certain illnesses or complications, the HPA axis will develop and function normally. However, certain physiological conditions can cause an abnormal HPA system reaction. Prolonged or intense stress or trauma can have the same result.
Heim et al. (2000) found that women sexually abused during childhood had higher levels of HPA responses to stress. The finding suggests that CRH hypersecretion, which leads to hyperactivity of the hypothalamic-pituitary-adrenal system, is a consequence of childhood abuse.
Newcomer et al. (1999) gave participants either high cortisol levels to produce blood sugar levels similar to those undergoing major surgery or lower cortisol levels similar to those undergoing minor surgery. The participant’s given high cortisol levels were worse at recalling prose passages, which shows the effects of stress on the hypothalamic-pituitary-adrenal system on memory.
Kiecolt-Glaser et al. (1984) took blood samples from 75 students one month before their examination (control condition) and on the first day of their exams (an experimental stress condition). They also completed questionnaires about levels of loneliness, number of life events and psychiatric state. They found the activity of natural killer (NK) hormone and T cells, which help fight infection, were lowered in the stress condition.
These studies show that those with higher stress hormone levels and those who have experienced significant trauma may develop a compromised HPA system function.
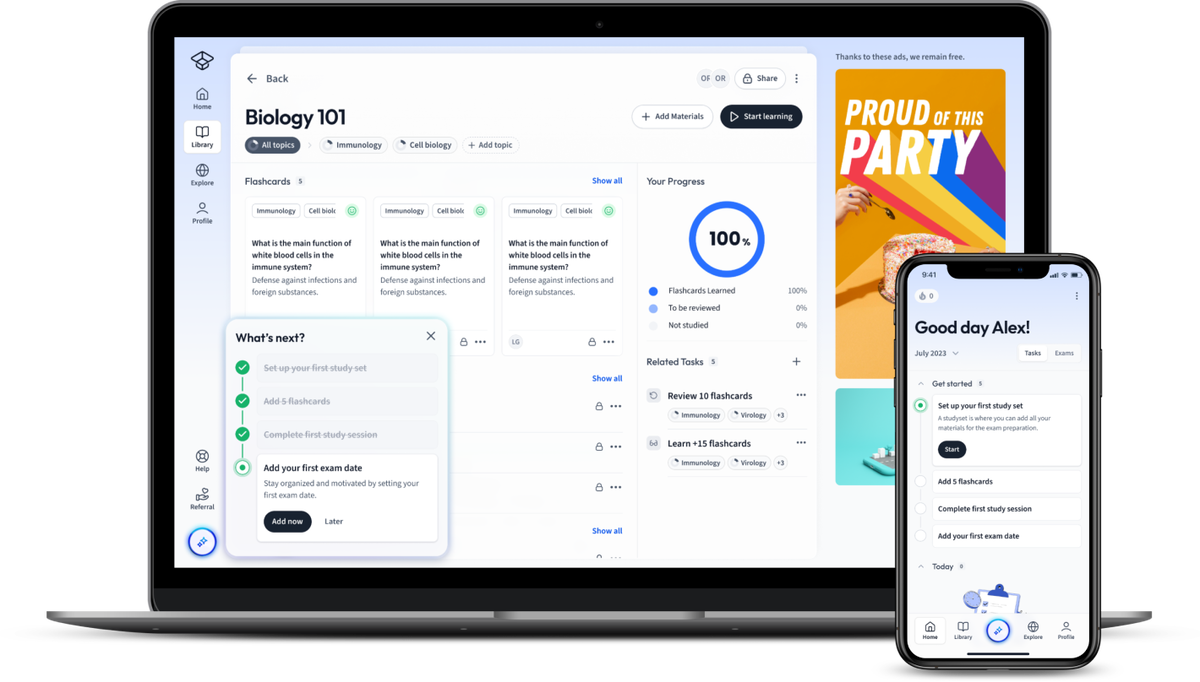
 Fig. 2 - Research has shown the negating effects of stress.
Fig. 2 - Research has shown the negating effects of stress.
Hypothalamic-Pituitary-Adrenal System: Depression
Stress affects our mood and contributes greatly to the development of depression. Our HPA system manages a cascade of stress hormones, so it’s no surprise to find that HPA dysfunction contributes to depression.
If a person experiences chronic stress, the HPA system is always activated, leading to excess cortisol. The cortisol receptors become desensitised, leading to noradrenaline and serotonin transmission disturbances.
Noradrenaline and serotonin are important in the regulation of mood and emotional behaviour.
Increased cortisol from an overactive HPA axis results in hyperactivity in the amygdala, an area of the brain responsible for regulating our emotions. This can lead to a reduction in serotonin production, which leaves us more vulnerable to depression and the effects of stress.
Studies have linked an overactive HPA axis with depression and major depressive disorder (MDD).
An overactive HPA system and depression can have physical consequences as well. Loneliness and problems such as depression are associated with a decreased immune system.
Kiecolt-Glaser et al. (1991) assessed depression, immune function and health in a group of people caring for a relative with Alzheimer’s disease (long-term stress group) and a control group. The stress group had significantly lower immune system functioning and higher instances of infectious illness and depression.
Hypothalamic-Pituitary-Adrenal System: Stress
Research has highlighted the importance of the HPA system in adaptive human behaviour. People who have their adrenal glands surgically removed need hormone supplements to combat stressors. This shows the vital role of the HPA system in dealing with stress. However, an overactive HPA axis can adversely affect our health and well-being.
When we encounter a stressor, our bodies react in a way that best prepares us to handle the immediate situation. Stressors trigger our body’s fight-or-flight response, amping us to face a threat (fight) or flee from it (flight). Our bodies do this by releasing adrenaline. Our muscles engage, and our heart rate and breathing increase, so we are better equipped to handle the threat.
As we saw above, stressors trigger our HPA axis, resulting in a release of cortisol. Most cells in the body have cortisol receptors. So while cortisol is a stress hormone, it plays an important role in bodily functions.
Cortisol controls many things, such as blood sugar levels, metabolism regulation and salt-water balance.
Our bodies need a balanced level of cortisol to function properly. An overactive HPA axis compromises this function by flooding our system with a constant supply of excess cortisol.
Prolonged exposure to chronic stress has negative effects on health, suggesting the HPA system may be wearing us down and hindering survival. This is because our stress response is old; it reacts the same way it would have done thousands of years ago. Now, it may not be equipped to deal with the modern stressors we face today.
Hypothalamic-Pituitary-Adrenal System: Dysfunction
While a little bit of stress is normal, chronic stress is not good for your health. If the stress system is always activated and the body cannot relax, it will lead to prolonged cortisol effects, negatively affecting health. HPA system dysfunction can also result from genetics (control factors such as cortisol response), biological causes (e.g., glucocorticoid medications) and childhood trauma. Effects of HPA system dysfunction include:
Anxiety and depression.
Digestive problems.
Headaches, muscle tension and pain: muscles in the body are in a constant state of guardedness against injury and pain.
Heart disease, heart attack, high blood pressure and stroke.
Sleep problems.
The hypothalamic-pituitary-adrenal system, which produces cortisol, plays a vital role in the sleep cycle. Cortisol has a 24-hour rhythm that controls sleep; this rhythm is disrupted due to chronic stress.
Weight gain: Your cells need energy, which causes your body to signal the brain that you are hungry and need to eat.
Memory and concentration impairment.
Glucocorticoids, including cortisol, play a role in regulating the immune system and reducing inflammation. Chronic stress (excess cortisol) can impair communication between the immune system and the hypothalamic-pituitary-adrenal system. As a result, several health conditions, such as diabetes, obesity, depression and immune disorders, may ensue.
Hypothalamic-Pituitary-Adrenal System - Key takeaways
The hypothalamic-pituitary-adrenal (HPA) system is the body’s response to chronic stress.
There are 5 phases to the HPA-axis stress response process.
Excessive stress contributes to depression and reduced immune system function.
Excessive cortisol can result in diminished memory and concentration and essential physiological processes dysfunction.
While the hypothalamic-pituitary-adrenal system is vital in dealing with stress, it is also maladaptive due to the consequences of chronic stress.
Explanations
Exams
Magazine